Battling Myelofibrosis & Finding Hope with a Bone Marrow Transplant
The story of Cindy, a 56-year-old teacher and single mother from Mount Juliet, Tennessee. She has lived with myelofibrosis (MF) for over six years, and began the bone marrow transplant process in 2022.

Everybody’s MF is different. This story does not constitute medical advice. Please talk to our doctor about your specific case. Participants featured have received compensation as a paid participants for Sobi.
An unexpected blood cancer
In a cold, colorless examination room in Nashville, Tennessee, Cindy first heard the words, “You have cancer, and if you don’t do something, you could die from it.”
She sat very still when the MF specialist left the room. Cindy had been diagnosed with myelofibrosis, a rare form of blood cancer. She couldn’t bring herself to stand up. Her body felt heavy, her feet glued to the floor. Slowly, she tried to grapple with what she heard.
Then, she composed herself, stood up from her chair, and walked out. Cindy was devastated. She hadn't understood the gravity of her disease. When she was first diagnosed, her primary care doctor hadn’t referred to her condition as cancer: she only knew she might have something called polycythemia vera (PV).
It had happened after an annual checkup. Cindy’s primary care doctor, who was her neighbor at the time, received her blood work at home one evening. He knew right away there was an issue: there were more red blood cells than normal.
He called Cindy that night. “I’d like to come over and talk to you about your results,” he said. “No,” she replied. Cindy knew something was wrong, and she wasn’t ready to hear it. Especially as a single mom with two daughters in school. Eventually, she complied, and her doctor came over and told her what he saw, referring her to another physician who confirmed the diagnosis.
Telling family she had a chronic, progressive disease was hard, she says. She told her sister first, but couldn’t bring herself to tell her parents. So, she didn’t. A few days later they all attended a family wedding rehearsal. There, her brother-in-law walked up to her, “How did your test go?” he asked, in front of her other sister who hadn’t heard the news yet.
Cindy’s heart started to beat quickly. She didn’t want to have this conversation before the wedding. But it was too late. She had to break the news to everyone. First to her sister, then to her parents.
Cindy knew something was wrong, but she wasn’t ready to hear it.

Battling Myelofibrosis & Finding Hope with a Bone Marrow Transplant
Facing progression of polycythemia vera to myelofibrosis
As Cindy’s disease was progressing, she knew her current doctor may not be able to help her as much as she needed. She had also discovered that her condition had moved from polycythemia vera to myelofibrosis – a bone marrow cancer that could potentially become acute leukemia one day. Cindy’s doctor was not a specialist in MPNs, or myeloproliferative neoplasms (cancers that start in the bone marrow,) so Cindy knew seeing a specialist would be beneficial.
Cindy decided to see Dr Michael Savona, a myeloid biologist and physician taking care of patients with chronic myeloid disease. “It was a godsend to have an MPN specialist in the area,” Cindy says.
Myelofibrosis is an incredibly rare and complex disease that manifests very differently in every person. Having the added support of an MPN specialist who is armed with the latest research available, is especially valuable for patients like Cindy whose disease has progressed to myelofibrosis.

Dr Savona and Cindy
Having the added support of an MPN specialist is especially valuable for patients.
Cindy developed a strong relationship with Dr Savona over the course of her treatment. Until her transplant, they had worked together for over five years.
From the start, Dr Savona was impressed by Cindy’s organization. After her diagnosis, she knew she wanted to keep everything documented in a binder. The binder helps organize her questions and her family’s questions, too, she says. She uses it to keep all documentation from her doctor visits, and she brings it to every appointment. “About 50% of the binder is my own research and 50% is information from my appointments,” she says. “I usually read articles on the MPN Research Foundation and Leukemia and Lymphoma Society websites ... and I would have a lot of questions,” she added.
“I don't think I ever remember her forgetting her binder,” Dr Savona says.
“This is really ideal, because sometimes patients will come from another doctor and have labs that didn't make their way to me and get faxed in. She has all that. Sometimes she even makes graphs of her lab work, so I can actually see trends. That's what you really want to see from patients, when they're making a real investment in their own healthcare.”
As she considered the possibility of a bone marrow transplant (the only cure for myelofibrosis,) she also began seeing new specialists. “But Dr Savona’s office is still right down the hall,” she says, which is a comfort.

Dr Savona and Cindy
“It can be hard to switch doctors. But it’s important to partner with a doctor who specializes in your disease.” — Cindy

A feeling that something just wasn’t right
How the ASXL1 mutation changed Cindy’s disease
After Cindy’s initial diagnosis, apart from itching, she didn’t have many symptoms until one day she noticed a weird feeling in her abdomen. She had pain under her ribcage and a persistent feeling that something wasn't right. Dr Savona immediately prescribed medication to reduce her spleen size, because it had been pushing against her ribcage, causing her discomfort.
For several years, the medication helped. But then, all at once, the discomfort, pain, and fullness in her stomach returned. She went back to adjust her medication.
“I knew right away when I started having that feeling in my ribcage… the pressure from my spleen. And for a long while I would think I could just adjust my posture and that it would help it go away. But in the back of my mind, I knew this was a change and that it was time I needed to see my doctor. Something was different.”
“It’s so important to stay in tune with your symptoms, your body and notice any changes.” — Cindy
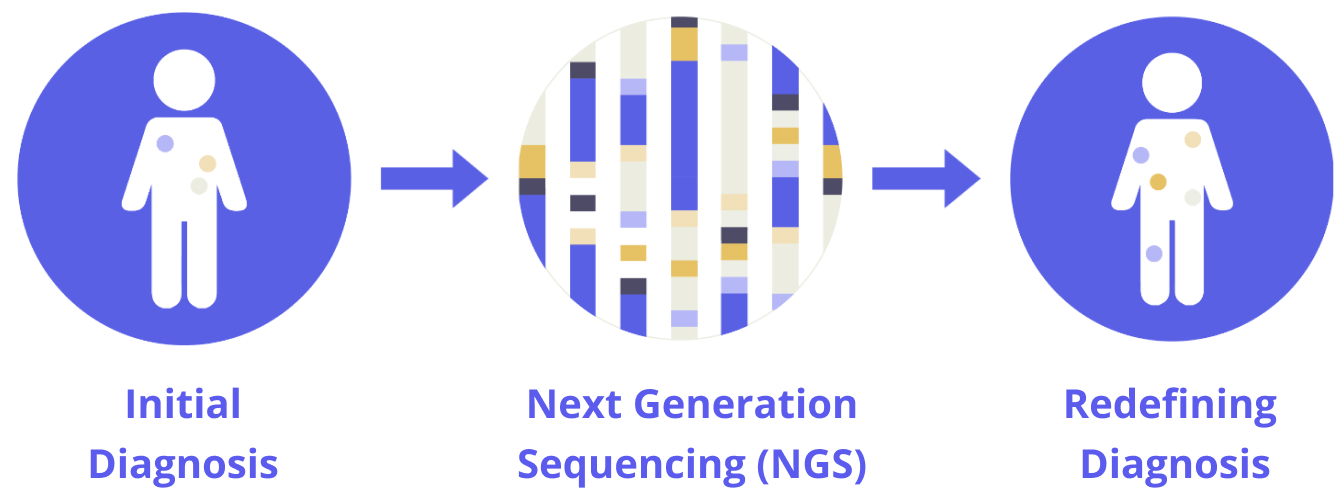
Not only was she experiencing discomfort, she also found that she felt full, even though she was eating much less food: a common symptom of an enlarged spleen. She immediately knew her disease had changed again and that her medication might have stopped working. She went back to see Dr. Savona, and right away he ordered a new genetic test, a next generation sequencing (NGS) panel, to see what might have changed in her body.
Essentially, an NGS panel looks for mutations in our DNA, quickly sequencing dozens of genes or whole genome. Because of this test, Dr Savona was able to identify a dangerous increase of an ASXL1 mutation in Cindy’s DNA – the level of ASXL1 in her body had tripled in a year. ASXL1 is an aggressive mutation that can accelerate into acute leukemia, and Dr Savona warned Cindy that she needed to act now.
“Anytime that I've gone to the doctor or sent them a message saying that I think my spleen is enlarged, they immediately take that as a change in your disease and will react,” Cindy says. “It’s so important to stay in tune with your body and notice any changes.” For Cindy, monitoring the changes in her body kept her alive.
“I knew this ASXL1 mutation was a huge change and that it was time to see my doctor.” — Cindy

The right time to take the next step
Preparing for the bone marrow transplant
Over the summer of 2022, free from her work as a teacher and with both daughters out of college, Cindy decided it was the best time to receive a bone marrow transplant – the only cure for myelofibrosis.
Bone marrow transplants for cancer patients are tricky to navigate and few are able to receive one. You have to be sick enough to need it, but well enough to undergo the transplant and survive. Several studies have shown that survival rates after myelofibrosis bone marrow transplants can be anywhere from 40-60%. And, bone marrow transplant success is not guaranteed once completed and, finding a donor for the transplant can also be challenging.
If no siblings or other family members are a donor match, it is often extremely difficult to find a donor. Fortunately, Cindy’s older sister was a match.“I feel obligated to her for the rest of my life,” Cindy says. “Because she was also my caretaker, along with my daughters.”
Together, they took turns caring for Cindy during the 100-day process. Her sister would drive from Alabama to take care of her three days a week, and her daughters would fill in the rest of the week. “They gave up their lives,” Cindy says. “During my recovery they just had to really be selfless because I struggled so much with what I wanted to eat and every day they were running to the store constantly to try to figure out what I would eat,” she added.
Since the transplant, Cindy’s oldest daughter Savannah continues to ask her mom to text her before she goes to bed every night to make sure she’s okay. “Last night Savannah called me at midnight while I was sleeping because I forgot to text her before I went to bed,” Cindy says. “She really worries about me.”

Cindy with her sister, who was also her donor
Are you looking for a marrow donor? Visit BeTheMatch.org for information.

Finding my purpose every day
Surrounding myelofibrosis with community
Myelofibrosis can be incredibly isolating. Many people don’t know what to say or do when a friend or loved one is diagnosed. And when you have myelofibrosis, it can be hard to explain to others, because the outward signs of the disease are often subtle. Even others who have myelofibrosis often have different symptoms than the ones you are experiencing because the disease presents itself in many ways.
“Some days, when I’m alone, everything starts to feel really heavy. Although I have purpose in my life and my days are full of wonderful people, I do have my times when I just fall apart for a minute. Maybe it’s on a walk in the woods, or maybe it’s when I’m in bed at night, but I do have tough days. When that happens, I know that as long as I'm still here, there's a purpose for me. I just take every day one step at a time,” Cindy says.
But “because people see me live a fairly normal life, I think everybody just kind of puts it aside,” she added. “So it's not until the next bone marrow biopsy where you get the big lab report, then you have to discuss it all over again. And with every few tests, there can be progression and that's when I have to have the conversations all over again. It's scary for me. It's scary for everybody.”

Cindy and her two daughters got matching tattoos that represent their close bond
“It’s important for people living with myelofibrosis to know that it’s more than physical. So much is mental.” — Cindy
“I think it's important for people to know that it's more than what's happening physically to you,” she added. “There's so much of it that's mental. Because I'm not going to the doctor every day, because I have my hair, people think I'm not sick. They expect to see me be sick. It’s so hard that people don't understand it. I didn't understand it and I wouldn't understand it if I weren't living in the middle of it. Because I don't look sick, people just can't wrap their heads around it.”
Being around people who do understand what she’s going through has been so important to her, she says.
Every Sunday, Cindy spends time with a Sunday school group of women. “We are very close – we constantly text, [submit] prayer requests, and are always on each other's minds, taking care of each other,” Cindy says. One woman at her church even helped organize and lead donor drives for her. “She just took that on, all on her own.”
“They are there for whatever I need. If they have to be the one that takes me to the doctor, if we need food, whatever, the yard mowed, someone in the church will come and mow the yard. My pastor has always been there. When I get the reports of a change in a [blood count] number, he's the first person I call and he kind of gets me through it before I call the rest. [Once], I made a trip to another hospital for a second opinion and I paid nothing for it. I had friends who donated their points for my flights because my older sister needed to go with me. I had friends who donated money for the rental car. I was given money to cover my meals. My sister paid for my hotel. Everything was covered. At the school where I work, the principal has also said, "We're here, whatever you need." Cindy’s physicians, friends, and family are always there to help – every step of the way.

Cindy’s group of work friends
Cindy’s physicians, friends, and family are always there to help – every step of the way.
Now, Cindy's life may change entirely. Her recent bone marrow transplant has the potential to erase myelofibrosis from her body altogether. If Cindy’s blood count stabilizes over time, she may finally be cured. No more blood transfusions, no more hospital visits, and no more expensive flights to fight her disease. She may finally be free from the grip of myelofibrosis.