A Self Portrait of Persistence
A Self Portrait of Persistence
8
min read

The importance of mental health support for myelofibrosis caregivers
Information displayed on this website is upon the condition that the persons receiving the same will make their own determination as to its suitability for their purposes prior to use or in connection with the making of any decision. Neither CTI BioPharma, its affiliates, nor their officers, employees, or agents shall be liable for any loss, damage, or expense arising out of any access to, use of, or reliance upon this website.

Dropping off a casserole. Running an errand. Helping out with a doctor appointment. We’re usually pretty good at supporting people we love through a short-term illness or injury. But with a disease like myelofibrosis (MF), caregiving is very different, according to licensed psychologist Dr Teresa Young, PhD. “When someone is going through a chronic illness for a period of time,” she said, " that’s a form of chronic stress [for the caregiver], a prolonged, sustained shift in roles.”
Young, who works with both patients and families struggling with chronic illnesses, spoke about some of the challenges of the caregiving role. Stress comes from the time-intensive requirement of caregiving, which adds to the initial shock of the patient's diagnosis. “If your caregiving relationship happens really quickly, you might not have thought very strategically about how to manage it, and that can create a lot of stress,” said Young. We asked Young and other experts to share more about how caregivers can sustainably offer support.


Dr Michelle Flaum, EdD, LPCC-S, DCMHS Professor Department of Counseling at Xavier University, said she focuses a lot on self-care with her clients who are caregivers. “Oftentimes they push back when it comes to addressing their own needs and taking care of themselves because the priority is the person they are providing care for,” she said. “[But] if people aren’t taking care of themselves and utilizing a support network, they’re going to be no good to the person they are caring for.”
Caregivers also deal with their own feelings about their loved one’s illness. Psychotherapist Marjorie Grafton, LISW-S, said, “Caregivers often carry the weight of cancer treatment in a way that can feel invisible. When you spend so much time and energy caring for another person, it can be hard to acknowledge that you also have your own grief, depression, and anxiety to work through,” she said.

In addition to the basic needs of self care, specialists suggest that caregivers take part in support groups, personal therapy, or family therapy. These structures can provide a broader perspective on what a patient goes through. In turn, reducing stress for the caregiver. “Sometimes caregivers aren’t familiar with how bad the patient feels,” said Young. “Maybe they can’t see that the person feels nauseous or fatigued. Providing that education can reframe how they think about the recipient.”


Another benefit to supporting the caregiver is making the patient feel more at peace. Young explained that, “For some people who are sick, they want their loved one to keep living their own life. It increases their sense of burdensomeness if the caregiver gives up everything. [The patient] wants to hear the story that you went out for coffee or took a cooking class. That can bring relief to patients.”
Ultimately, mental health support for MF caregivers is good for everyone. Grafton said, “The more that caregivers receive their own support, the better they are able to be in a relationship with the cancer patient that they love, improving the quality of their relationship as well as improving health outcomes.”
While much can be gained from traditional, in person, one-on-one sessions with a therapist, they may not be right for everyone. In recent years, due in part to the pandemic, a variety of online and offline options for mental health care have become more accessible. Our experts recommend exploring both clinical support and other activities that may give caregivers a replenishing break—a moment, an hour, or a day, where they can recharge themselves.
Psychotherapist Grafton provided a list of what caregivers should notice in their own lives when deciding whether to seek help:
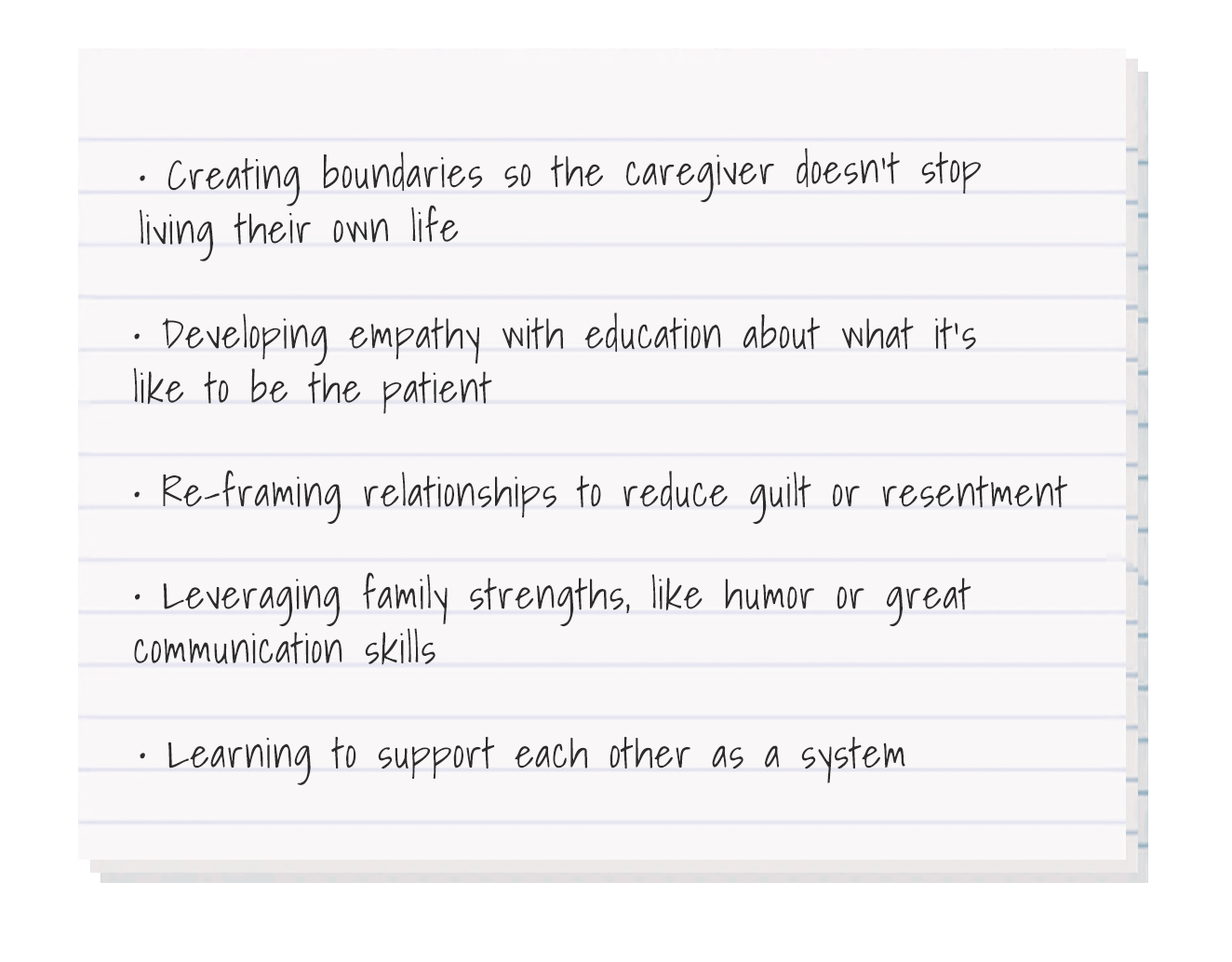
Psychologist Young said family therapy is a great way for patients to talk about their experiences and caregivers to talk about their fears together, in a structured setting. Some of the benefits you might experience getting help together: